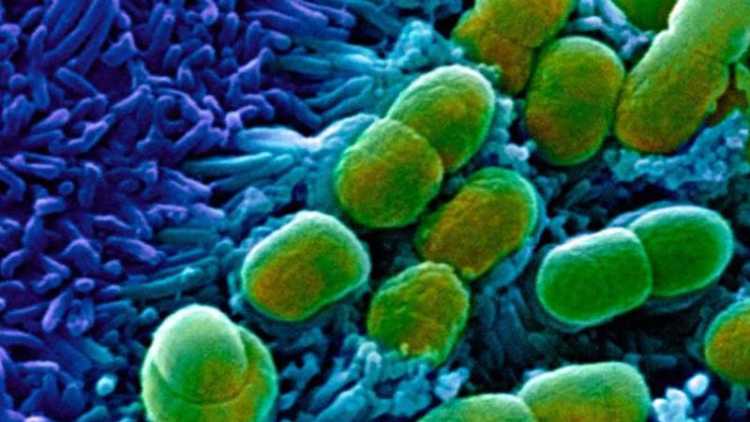
Artificial intelligence has been used to discover new antibiotics effective against untreatable diseases, marking the advent of a major new tool in the global fight against drug resistance.
In a paper published on Thursday in the journal Cell, researchers at the Massachusetts Institute of Technology reported the discovery of a potent new antibiotic, halicin, which was able to kill 35 powerful bacteria.
Among the pathogens targeted were Clostridium difficile, tuberculosis and Acinetobacter baumannii, an effectively untreatable infection often seen among US veterans, which enters wounds and frequently causes death.
“We are facing a global crisis, due to increased emergence of resistant bacterial pathogens that are rendering our current antibiotic arsenal ineffective,” said James J Collins, the biological engineer at the Massachusetts Institute of Technology who led the work.
“If we don’t address the crisis by 2050, the annual deaths due to antibiotic-resistant infections will grow to 10m, which is higher than the death rate due to cancer,” he added.
The new antibiotic was discovered using a deep-learning algorithm developed by computer scientist Regina Barzilay, which was trained to analyse the structure of 2,500 molecules, including current antibiotics and other natural compounds such as glucose, to determine their anti-bacterial potency.
The algorithm then scanned through a library of 100m molecules to predict how effective each would be against specific pathogens. It was also primed to seek out molecules that looked physically different from existing antibiotics, to avoid perpetuating the problem of resistance among the newly discovered compounds.
“There is still a question of whether machine-learning tools are really doing something intelligent in healthcare, and how we can develop them to be workhorses in the pharmaceuticals industry,” Ms Barzilay said. “This shows how far you can adapt this tool.”
Despite the scientific promise of molecules such as halicin, and eight others discovered by the MIT lab, market forces remain a big hurdle to their broader clinical rollout.
“We see many promising new ideas against drug resistance. [But] the key gaps today are economic, not just scientific,” said Kevin Outterson, a healthcare lawyer at non-profit Carb-X, who works on business models for antibiotic development.
One factor is that patients typically only take antibiotics over a few days or a week, whereas other drugs that are used over the course of many months or even a lifetime, but cost a similar amount to develop, can prove more cost-effective.
And even if an antibiotic does make it to the clinic, healthcare professionals are often disinclined to prescribe it because of fears over spreading bacterial resistance, while in the US, they can be financially incentivised to prescribe more expensive drugs.
However, the use of machine learning to accelerate drug discovery could bring down the cost of generating future antibiotics, while targeting currently untreatable diseases could open up lucrative new markets. “We could dramatically reduce the cost required to get through clinical trials,” Mr Collins of MIT said.